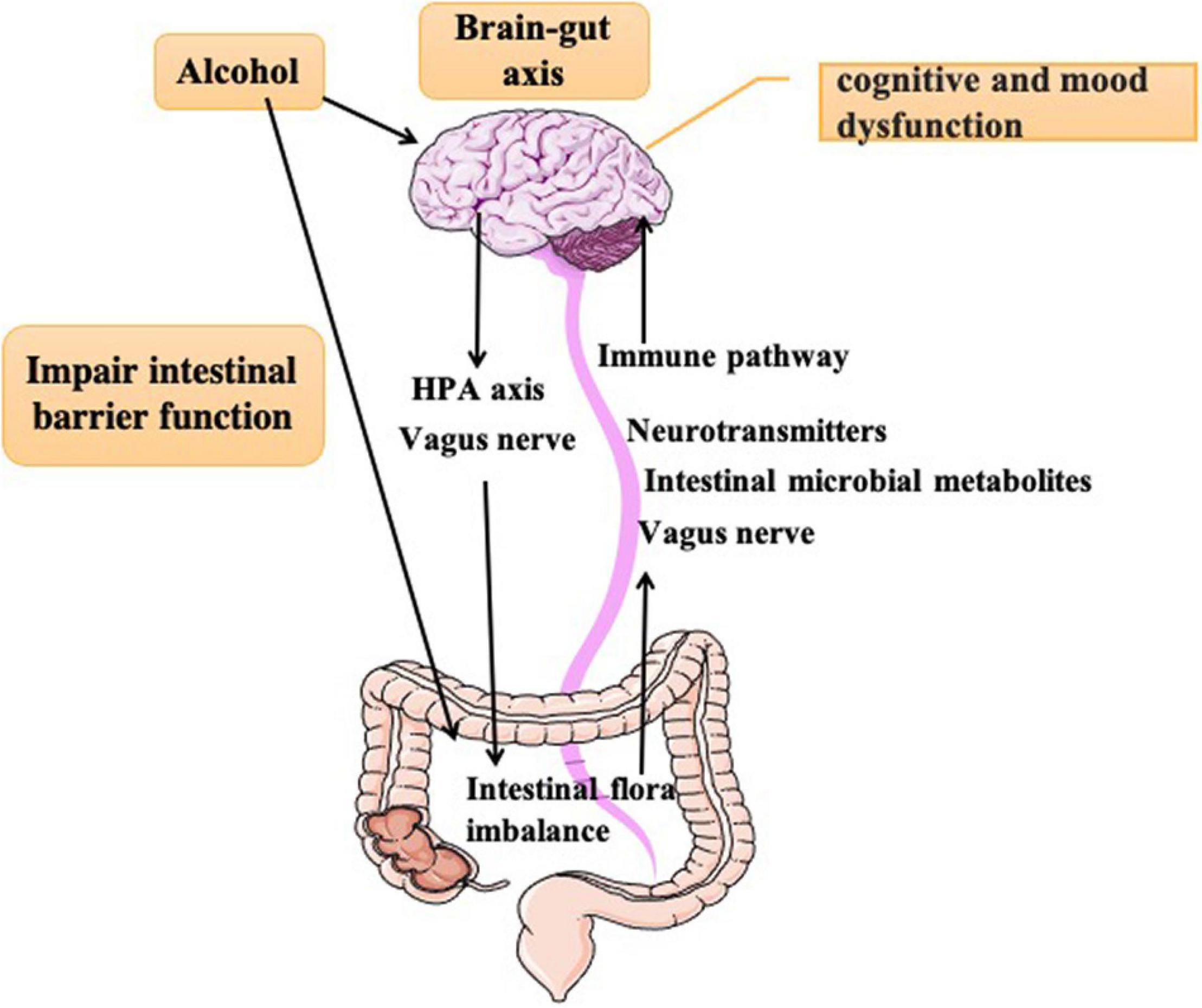
The human body is composed of complex systems that work together to maintain overall health and function. One of the most fascinating and intricate systems is the gut-brain connection, a bidirectional communication network between the central nervous system (CNS) and the enteric nervous system (ENS). The gut-brain connection allows for the exchange of information and molecules between the gut and the brain, influencing various physiological processes, including digestion, metabolism, and behavior.
Recent research has shed light on the importance of abdominal neurons in forming the gut-brain connection. A study published in the journal Nature Communications found that a specific group of neurons in the abdomen, known as the abdominal vagal neurons, play a crucial role in establishing and maintaining the gut-brain connection.
The abdominal vagal neurons are a subset of the vagus nerve, a complex nerve that extends from the brain to the abdomen. These neurons are responsible for transmitting signals from the gut to the brain, influencing various physiological processes, including appetite, satiety, and metabolism.
The study found that the abdominal vagal neurons are responsible for detecting and responding to changes in the gut microbiome, the trillions of microorganisms that inhabit the gut. The gut microbiome produces various metabolites, including short-chain fatty acids, which are detected by the abdominal vagal neurons. These neurons then transmit signals to the brain, influencing the regulation of appetite, satiety, and metabolism.
The findings of this study have significant implications for our understanding of the gut-brain connection and its role in overall health. The gut-brain connection has been implicated in various diseases and disorders, including obesity, metabolic syndrome, and neurological disorders such as Parkinson’s disease and Alzheimer’s disease.
Understanding the role of abdominal neurons in forming the gut-brain connection may lead to the development of new therapeutic strategies for these diseases. For example, targeting the abdominal vagal neurons may provide a novel approach for treating obesity and metabolic syndrome, by modulating the regulation of appetite and satiety.
Furthermore, the study highlights the importance of the gut microbiome in shaping the gut-brain connection. The gut microbiome is influenced by various factors, including diet, lifestyle, and environmental factors. Modulating the gut microbiome through dietary interventions or probiotics may provide a novel approach for influencing the gut-brain connection and promoting overall health.
In conclusion, the discovery of the role of abdominal neurons in forming the gut-brain connection has significant implications for our understanding of the complex relationships between the gut, brain, and overall health. Further research is needed to fully elucidate the mechanisms underlying the gut-brain connection and to explore the therapeutic potential of targeting the abdominal vagal neurons.