The world of virology and public health was recently shaken by the detection of a bird flu variant in Nevada dairy cows. Identified as a strain of H5N1 avian influenza, this variant has displayed genetic mutations associated with the ability to infect mammals, a development that experts view with concern. Its appearance in farm cattle not only surprises the scientific community but also poses critical questions about the containment of zoonotic diseases and potential impacts on public health.
Avian influenza is predominantly found in waterfowl and domesticated birds, rarely affecting mammals. However, in recent decades, sporadic cases of bird flu infecting mammals, including humans, have been recorded worldwide. These instances are often the result of genetic changes in the flu virus that enable it to overcome the interspecies barrier.
The variant detected in Nevada, researchers confirm, is distinguished by adaptations that facilitate effective replication in mammalian cells. Early reports suggest the virus was first identified in dairy herds, where unusual symptoms and disease patterns prompted local farmers to collaborate with virologists for testing. Studied samples revealed that while the virus is an avian strain, genetic sequencing shows mutations similar to those causing mammalian infections in past cases.
Public health agencies have raised alarms about the potential repercussions of this development. Cooperative investigations by the Nevada Department of Agriculture and federal authorities, including the U.S. Department of Agriculture (USDA), indicate the strain’s rapid spread among isolated dairy herds. Wildlife studies around the affected farms show evidence of massive die-offs of birds, suggesting wild species may have been the vector for transmission into cows.
This recent episode is reminiscent of previous global concerns during the H5N1 outbreaks in Asia and Europe, which led to widespread poultry culling and transport restrictions. However, experts underline that the emergence of such a strain in mammals adds complexities not witnessed before, as mammals could potentially act as bridging hosts for further mutations that might increase transmissibility to humans.
Laboratory studies conducted by the Centers for Disease Control and Prevention (CDC) reveal critical findings. Unlike traditional H5N1 strains, the Nevada variant has acquired the ability to bind more effectively to receptors in mammalian, including human, respiratory cells. While human-to-human transmission seems unlikely at this stage, authorities remain cautious about potential mutations if this variant continues to circulate unchecked.
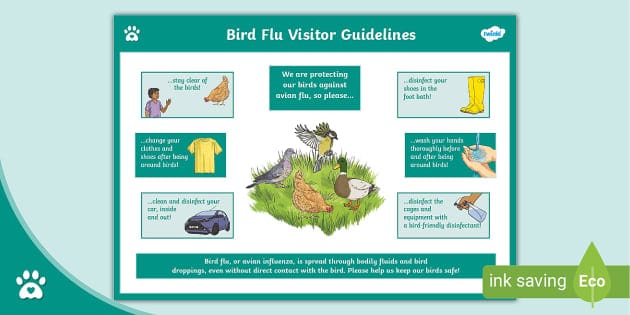
Already, precautionary measures are underway within the Nevada agricultural sector to protect livestock and workers from exposure. Farms have implemented rigorous biosecurity measures to prevent further outbreaks, including quarantining affected cattle populations, limiting animal transport, and intensifying monitoring. Public health experts urge that maintaining hygienic practices, strict compliance with occupational safety, and consistent veterinary checks are crucial to averting wider dissemination.
Addressing the risk to human populations, global organizations like the World Health Organization (WHO) and the Food and Agriculture Organization (FAO) are collaborating in investigations while preparing vaccine formulations for emergency use. Such preparation is part of a broader response framework aiming to contain the virus regionally while preventing international spillover.
Economically, the implications are significant as dairy farms bear losses related to diminished production, culling of infected livestock, and disruptions in trade. Domino effects could also extend to increased health costs and surveillance infrastructure investments, underscoring the interconnected vulnerabilities in agriculture and public health spheres.
While no human cases have been definitively connected to the Nevada outbreak yet, the international health community has not ruled out the possibility of isolated spillover events. Human infections in past outbreaks of similar strains have usually occurred through close contact handling or eating infected poultry. Consequently, the Nevada variant warrants careful monitoring, particularly for workers and communities living in close proximity to affected farms.
Understanding viral adaptation mechanisms continues to be pivotal for pandemic preparedness planning. Discoveries from this outbreak have sparked debates in research environments about the trajectory of zoonotic diseases and factors that escalate interspecies jump risks. Scientists warn that lessons applicable here must extend toward mitigating threats from other viral families, including coronaviruses, whose rapid mutation cycles present persistent challenges for long-term disease containment strategies.
The Nevada bird flu outbreak is a clarion call for global coordination between veterinary science, virology, and international policy. Continuous investments in surveillance technologies and vaccine development programs, alongside prioritization of transparent scientific communication, will be vital for controlling avian influenza and multi-species spillover risks.
As scientific teams work urgently toward containing the Nevada variant, the incident underscores the importance of adopting proactive systemic measures addressing the dynamic nature of zoonotic pathogens. It also reaffirms the fundamental understanding that patterns of interconnected ecosystems—where humans, wildlife, and livestock coexist—are at the heart of infectious disease emergence, demanding equally integrated global responses.